The Anterior Hip Replacement is an increasingly popular method of replacing a hip joint due to the benefit of not needing to cut or detach any muscle or tendon as part of the operation.
Not cutting tendon or muscle has many benefits, such as pain and quicker recovery. However, successful surgery depends on many other factors such as the quality of surgical components, surgical experience and training, as well as factors related to the patient.
Hip replacement surgery is major surgery with more than 49,000 procedures performed each year in Australia. It is a very successful operation and most hip replacements will last 20 – 30 years.

Hip replacement
The hip joint is a ball and socket joint, made up of the femoral head (ball) and the acetabulum of the pelvis (socket). During a hip replacement, the femoral head and acetabulum are replaced with a titanium femoral stem and a titanium socket for the acetabulum. A femoral head is then placed on the titanium stem, which is made of either chromium cobalt or ceramic, whilst a liner is placed in the acetabulum, which can be made of polyethylene plastic or ceramic.
Anterior approach
The primary goal of Anterior Hip Replacement is to minimize harm to muscles, blood vessels and nerves surrounding the joint. It is a technique designed specifically to achieve these goals as it is a true muscle-sparing surgical technique
The potential benefits from the anterior approach include:
-
Preservation of Muscle
As the anterior approach of the hip goes in between the muscles in the front of the hip, without the need to cut any muscles or tendons. The 2 most common traditional methods, called the Posterior and Lateral Hardinge approach, require releasing muscles and tendons off the femoral bone. These tendons are then reattached at the end of the procedure
-
Prevention of limping
By preserving the muscle, patients are less likely to develop long term problems such as a limp, which can occur after the gluteal tendons are detached from the top of the femoral bone, such as in the lateral Hardinge approach
-
Post-operative pain
In conjunction with modern anaesthetic techniques, patients experience much less pain with hip replacement surgery
-
Reduced risk of hip dislocation
(separation of the hip ball and socket): By preserving the muscles around the hip, the stability of the hip is greatly improved. The risk of dislocation is minimal. Also, the post-operative limitation of movements, usually necessary with the posterior and lateral techniques, is no longer necessary. The risk of dislocation is reduced because the Anterior Hip Replacement technique is performed from the front of your body and dislocation is mainly related to damage the structures around the back of the hip.
-
Rehabilitation and Recovery
Rehabilitation starts on the day of the operation. Standing up and walking with arm-crutches or a walker can begin immediately. Research has shown that patients recover quicker with the anterior approach.
-
Small skin scar
The Anterior approach of the hip is performed through a small incision in the front of the hip usually 6 – 10cm long
-
Hospital stay
Most patients go home after 3 days after the operation with minimal pain and walking comfortably
Outcomes
It is important to understand what an anterior hip replacement can and cannot do before deciding to undergo the operation.
Most people who have anterior hip replacement surgery, experience a dramatic reduction in hip pain and a significant improvement in movement.
With almost 70 years of history, hip replacement surgery is a very common and safe procedure for the treatment of severe osteoarthritis.
The main benefits of a successful total hip replacement are:
- Reduction in hip pain: your pain will be rapidly and dramatically reduced
- Recovery of mobility: your hip will function with less effort, almost regaining your original mobility.
- Improvement in quality of life: your everyday activities and your social life will no longer be limited by your hip pain and stiffness.
However, there are certain things that you cannot do with an anterior hip replacement. Such as
- long distance running
- any high impact sports such as football

The right hip has a Total Hip Replacement and the left hip is normal.
Reasons for Surgery

The Right Hip has been affected by Osteoarthritis
The Anterior Total Hip Replacement is for patients who have severe pain and stiffness in the hip.
Reasons to replace a hip
The most common reason to replace a hip is arthritis. There are many causes of arthritis, but the most common ones include:
-
Osteoarthritis
Usually affects people above 50 years old but can affect younger people. It is essentially a ‘Wear and Tear’ process affecting the cartilage of your hip. Cartilage covers the bones of your hip joint, the femoral head (ball) and acetabulum (socket). As you age, your cartilage wears down, causing hip pain and stiffness
-
Rheumatiod arthritis
Is an autoimmune disease in which a special membrane in your hip joint, called the synovial membrane becomes inflamed. This inflammation damages the joint cartilage.
-
Osteonecrosis
Your hip joint can be affected by a condition called osteonecrosis or bone death. There are many possible reasons for osteonecrosis which include prolonged steroid use, alcohol abuse or genetics
Is Surgery for You?
Whether to have hip replacement surgery should be a joint decision made by:
- yourself
- your family
- your GP
- Professor Phong Tran.
You should consider
- the pros and cons of the operation,
- the possible complications
- alternative treatments other than surgery
- the surgical options
You may benefit from hip replacement surgery, if:
- Your hip pain is severe
- It limits your movements and activities such as walking
- It impairs your ability to look after yourself such as with showering, putting on shoes and socks.
- The pain is present at night and at rest.
- You have tried non-surgical alternatives without success

Nonsurgical Options
- Hip replacement surgery should only be considered after trying other options that don’t involve surgery.
- These include
- pain-relieving medications
- physiotherapy
- weight loss
- walking aids such as walking sticks.
Day of Surgery
Admission
Most people are admitted to the hospital on the day of surgery.
Anaesthesia
The anaesthetist will see you and decide the type of anaesthetic that’s best for you.
The different types of anaesthesia include:
- General Anaesthetic. This type of anaesthetic puts you asleep during the whole procedure and a machine controls your breathing.
- Spinal Anaesthetic. An injection is placed into your back to numb your hip and legs. You will be awake during the procedure, however, a sedative can be given to you to help you doze off.
- Nerve Blocks. This special injection is used to help with your pain after the operation and is often used in conjunction with a general anaesthetic.
Operation
The operation usually takes between 1 to 2 hours.
The damaged cartilage and bone are removed and replaced with a new hip replacement.
Your wound is usually about 10 long, depending on your shape and your hip anatomy, and is located directly in front of your hip.
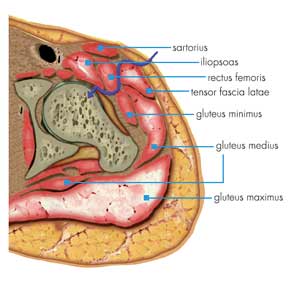
A gap between two of your hip muscles is used to reach your hip joint.
The arthritic femoral head (ball) is removed. Your acetabulum (socket) is then prepared for the new implant.
The titanium acetabular cup is then secured into your hip joint socket. Inside this cup will be a liner made of either ceramic or highly cross-linked polyethylene.
Your thigh bone (femur) is then prepared and your new titanium femoral stem is then inserted. The femoral ball is then placed on top of the titanium stem, which is made of either ceramic or chromium cobalt.
Your hip joint is then tested for stability, flexibility and size.
During the operation, an x-ray machine called “fluoroscopy” will be used to check your component placing, making sure you have the right size components and then everything is placed in the best position.

Anterior Hip Replacement
Prosthesis choices in the Anterior Hip Replacement
What is a Hip Replacement made of?
Hip replacements are made of either surgical grade metal (often chromium cobalt, stainless steel or titanium), highly wear-resistant plastic or ceramic.
A hip joint is basically a ball and socket joint, and a hip replacement is designed to replace this normal anatomy.
A hip replacement is composed of a:
- Socket: Medically called the Acetabular Component. It is usually made of titanium.
- Liner: The liner fits snugly into the socket to provide an ultra-smooth surface for the hip joint. It can be made of ceramic or plastic (highly cross-linked polyethylene)
- Ball: The artificial ball component is smaller than your normal hip ball. It is incredibly polished and perfectly round and smooth. It is usually made of ceramic or metal (chromium cobalt)
- Stem: The stem fits snugly into your thigh bone (femur) to provide a stable structure for the ball. It is made of titanium. The stem can either be used with or without surgical cement. With it is a stem without surgical cement, it is called “an uncemented stem” and has a special coating that encourages your bone to grow into and bond with the stem. A “cemented stem” is used when your bone is either weak with osteoporosis or the inside of your thigh bone (called the canal) is wide, and therefore better suited to an uncemented stem.
There are many types and shapes of hip replacements available, and Prof. Tran will decide which one is best for you.
Recovery Room
After the operation, you will be resting in the recovery room, where specially trained nurses will closely monitor you. This usually takes about 1 hour. After which, you will be taken to your room in the hospital ward.
Hospital Stay
The time you spend in the hospital depends on your individual circumstances and general health. Most patients will spend their time in hospital on either
- 1st Floor or 2nd Floor of St Vincent’s Private East Melbourne
- 1st Floor St Vincent’s Private Werribee
The average stay in hospital is 2-3 days, but if your general health is poor, then you may need to spend more time on the ward recovering or in rehabilitation. For your convenience, rehabilitation can be organised for the 5th Floor of St Vincent’s Private East Melbourne.
The golden rule is … you only go home after you are walking safely and your pain is well controlled. How long that takes is different for everyone.
The wonderful nurses and physiotherapists at St Vincent’s Hospital East Melbourne or Werribee will take the best care of you and tailor your stay to your needs.
Pain
The pain after an anterior approach hip replacement is usually rated by patients to be around 3 out of 10. Most patients have a spinal anaesthetic which keeps the legs numb and painful for a few hours after the operation. Pain killers are prescribed to help keep the discomfort to a comfortable low level.
Walking
Most people can start gently walking on the day of surgery. During your stay in the hospital, you will increase the distance you walk and the time you spend on your feet.
Bruising and Swelling
It is not uncommon for your thigh to become quite bruised and swollen. It can sometimes look very severe and also include your knee and calf. This is due to the effect of gravity and usually quite normal. However, if you develop pain in your calf, it is very important to seek medical help as soon as possible, as you might be developing a DVT (blood clot in the leg), which can be a potentially very dangerous condition.
Preparing for Surgery
Tip
Carry a list of your medications with you including the name, dosage and how often you take them.
Before your operation, your fitness for the operation will be assessed by our perioperative physician or Anaesthetist. There will be a number of tests performed in preparation for the operation.
Tests
Tests that may be ordered for you include:
- blood tests
- ECG
- CT scan of your hip to help prepare the correct size and shape of your hip replacement
Preparing Your Skin
Your skin should not have any infections or irritations before surgery. If either is present, contact us.
There is no need to shave before the operation, as we will prepare your skin on the day.
If you do choose to shave your skin before the operation, do it 1-2 weeks before surgery so that there are no skin reactions or rashes. Sometimes, your operation will have to be delayed if the skin is not perfect on the day of surgery.
Medications
Your perioperative physician or Anaesthetist will advise you on which medications you should stop or can continue taking before surgery.
Go see your dentist
Consider getting treatment for significant dental diseases (including tooth extractions and periodontal work) before your hip replacement surgery. Routine cleaning of your teeth should be delayed for several weeks after surgery.
Get some help from your friends and family
Although you will be able to walk with crutches or a walker soon after surgery, you will need some help for several weeks with such tasks as cooking, shopping, bathing, and laundry. If you live alone, our office can help you make advance arrangements to have someone assist you at your home or an ongoing stay at Rehab can be arranged.
Home Planning
Most patients do not need any home modifications.
However, if you are having trouble then the following is a list of home modifications that will make your return home easier during your recovery:
- Securely fastened safety bars or handrails in your shower or bath
- Secure handrails along all stairways
- A stable chair for your early recovery with a firm seat cushion (that allows your knees to remain lower than your hips), a firm back, and two arms
- A stable shower bench or chair for bathing
- A long-handled sponge and shower hose
- A dressing stick, a sock aid, and a long-handled shoehorn for putting on and taking off shoes and socks without excessively bending your new hip
- A reacher that will allow you to grab objects without excessive bending of your hips
- Firm pillows for your chairs, sofas, and car that enable you to sit with your knees lower than your hips
- Removal of all loose carpets and electrical cords from the areas where you walk in your home
Exercises before Surgery
Recovery and Rehabilitation
How do I look after my wound?
It is important to keep your wound as dry as possible.
Most patients are discharged home with a waterproof dressing, which can be left on for showering.
During the first 24 hours, it is normal to have some minor bleeding. After being discharged home, there should be no discharge, redness or bleeding around the wound.
If there is redness, discharge or a foul odour, please seek medical attention as soon as possible.
When will my stitches be removed?
Your wound is closed with a dissolvable stitch and surgical glue is used to seal the wound. Therefore, there are no sutures or surgical clips that need to be removed after the surgery.
When you go home, your wound will have a white waterproof dressing that you can shower with. About 1 week after surgery, you will remove the white waterproof dressing and underneath it is a glued-on mesh dressing (which is clear) which you will keep on for another 7 days. This mesh dressing is also waterproof, and you can have showers with it.
After that 7 days, you can peel off the mesh dressing yourself, and after that, you should be able to have baths, swim or perform hydrotherapy.
What should I eat and drink?
There are usually no specific diet or extra vitamins/nutrients needed to recover from a total hip operation.
It is important to have a normal healthy balanced diet and plenty of nonalcoholic fluids.
If your Body Weight Index is over 40, then you should endeavour to lose weight before the surgery. Patients with a BMI over 40, have an increased risk of surgical infection and complications.
What exercises should I do at home?
Physiotherapy and the exercises that you perform at home are extremely important to achieve the best results after a hip replacement.
After returning home, you should gradually be able to do more and more. It is important to look after your new hip and follow Prof. Tran’s and physiotherapy instructions.
Your program may include exercises that work on your:
- walking
- sitting
- stair climbing
- muscle strength
Special Precautions
One of the possible complications of hip replacement surgery is dislocation. Fortunately, after the anterior hip replacement, dislocation is very rare. Because it is a muscle-sparing approach, there are no restrictions on the way you sit or cross your legs
Taking care of your new hip
Long term care of your total hip
DON’T FORGET:
- Lead a healthy and active life.
- In case of fever, throat inflammation, pulmonary inflammation or any infection, tell your doctor that you have a hip implant.
- be careful to not fall heavily onto your hip, as this can cause a fracture if the fall is severe enough
Avoiding Falls
A fall during the first few weeks after surgery can damage your new hip and may result in a need for more surgery.
Be careful on Stairs. Stairs are a particular hazard until your hip is strong and mobile, and you’ve regained your balance. You should use a walking aid such as a cane, crutches, a walker. Use the handrails on your stairs or ask for someone to help you., or handrails or have someone help you.
Complications and Risks
The complication rate following hip replacement surgery is very low.
However, it is important to always understand potential complications (no matter how small the risk) when considering any operation.
The risks for a total hip replacement include:
- Joint infection. Serious complications, such as joint infection, occur in fewer than 1% of patients.
- Heart attack and Strokes. Major medical complications, such as heart attack or stroke, occur even less frequently.
- Deep vein thrombosis (DVT) Blood clots in the leg veins or pelvis are the most common complication of hip replacement surgery. You will be prescribed one or more measures to prevent blood clots from forming in your leg veins including TED stockings, compression foot pumps, and blood-thinning medications.
- Uneven legs. Leg-length inequality after a hip replacement. Often this is temporary, as your muscles and soft tissues get used to the new prosthesis. Also, the prosthesis will settle in over time. Modern techniques such as CT Scan 3D modelling and planning, as well as the use of x-ray during the operation, significantly reduce this risk. If you do have a leg length discrepancy after surgery, then some patients may feel more comfortable with a shoe lift or insert.
- Dislocation. This is rare after a hip replacement is performed after the anterior approach.
- Loosening of the components. Over years, the hip prosthesis may wear out or loosen. This problem will likely be less common with newer materials and techniques. When the prosthesis wears, bone loss may occur because of the small particles produced at the wearing surface. This process is called osteolysis.
- Revision surgery – having the operation done again.
Blood Clots | Deep Vein Thrombosis | DVT
One of the main risks of having a total hip replacement is a blood clot formation in the legs called a Deep Vein Thrombosis (DVT). The danger with a DVT is that it may move to your lungs and cause severe and sometimes life-threatening breathing problems called Pulmonary Embolism (PE).
This threat is present anytime after your operation and lasts for several weeks after your surgery.
To reduce this risk as much as possible
Whilst in hospital, you will:
- wear special compression stockings
- use compression foot pumps
- be given daily injections or tablets of blood thinners called anticoagulants
- walking and exercise every day to help circulate your blood
Whilst at home
Look for the warning signs of DVT.
These include:
- Pain in your calf
Warning signs that a blood clot has travelled to your lung include:
- Shortness of breath
- Chest pain, particularly with breathing
Notify Prof.Phong Tran immediately if you develop any of these signs.
Preventing Infection
The most common causes of infection following hip replacement surgery are bacteria that enter the bloodstream during dental procedures, urinary tract infections, or skin infections. These bacteria can lodge around your prosthesis.
Following your surgery, you may need to take antibiotics before major dental work or any surgical procedure that could allow bacteria to enter your bloodstream.
Warning signs of a possible hip replacement infection are:
- Persistent fever (higher than 37.5°C orally)
- Shaking chills
- Increasing redness, tenderness, or swelling of the hip wound
- Drainage from the hip wound
- Increasing hip pain with both activity and rest
Notify Prof.Phong Tran immediately if you develop any of these signs.
FAQ's
-
What are the important things to look for after a hip replacement?
- Redness, swelling or warmth around the cut
- Leakage from the cut
- Fever and chills.
- Severe knee pain that is not relieved by prescribed painkillers.
- Sudden sharp pain and clicking or popping sound in the knee joint
- Loss of control over leg movement
- Loss of leg movement
-
Does Prof. Tran perform metal on metal hip replacements?
No. Prof. Tran has never performed this operation because of the high revision rates associated with some of the metal on metal hip replacements.
Also, there is significant concern regarding the adverse health consequences of metal particles and metal ions.
Reference
-
Does Prof. Tran perform the Birmingham Hip Replacement?
No. The Birmingham Hip replacement is a type of Metal on Metal Hip Replacement.
-
Will my hip replacement activate the metal detectors at airports?
Some hip replacements may activate metal detectors at airports and some buildings.
Patients have reported mixed experiences at airports. Most patients don’t find that they don’t set off metal detectors, but occasionally it can.
-
What exercises should I avoid after Anterior Hip Replacement?
Antibiotics are not necessary for most dental procedures including routine cleaning.
However, if there is infection or large dental procedures where infection is a risk, then a course of antibiotics is recommended.
-
Do I need to take antibiotics when I see the Dentist?
High impact activities such as:
- contact ball sports (eg football)
- long-distance running
- any sport that has a high risk of falling
References
- Australian National Joint Registry
- The Impact of Surgical Technique on Patient Reported Outcome Measures and Early Complications After Total Hip Arthroplasty. Sibia US, Turner TR, MacDonald JH, King PJ. J Arthroplasty. 2016 Nov
- Total Hip Arthroplasty Performed Through Direct Anterior Approach Provides Superior Early Outcome: Results of a Randomized, Prospective Study. Orthop Clin North Am. 2016 Jul;47(3):497-504.
-
MR imaging of soft tissue alterations after total hip arthroplasty: comparison of classic surgical approaches. Eur Radiol. 2017 Mar;27(3):1312-1321
- The monitoring of activity at home after total hip arthroplasty. Bone Joint J. 2016 Nov;98-B(11):1450-1454.
- Limited benefits of the direct anterior approach in primary hip arthroplasty: A prospective single centre cohort study. J Orthop. 2016 Oct 26;14(1):53-58.
- The Impact of Surgical Technique on Patient Reported Outcome Measures and Early Complications After Total Hip Arthroplasty. J Arthroplasty. 2017 Apr;32(4):1171-1175.
- Functional and clinical outcomes following anterior hip replacement: a 5-year comparative study versus posterior approach. ANZ J Surg. 2016 Jul;86(7-8):589-93.

