What is Hip Arthroscopy?
Hip arthroscopy is a form of keyhole hip surgery performed through small incisions to diagnose and treat problems inside the hip joint. Through 2–3 incisions (around 1 cm each), we insert a camera (arthroscope) and fine instruments to repair damage with minimal disruption to muscles and surrounding tissues.
Compared with open surgery, keyhole hip arthroscopy is less invasive, typically results in smaller scars, and supports a faster, staged recovery. It is a specialised procedure performed by surgeons with advanced fellowship training and high-volume experience.

What conditions can be treated by hip arthroscopy?
Hip arthroscopy allows us to visualise and treat a range of conditions inside the joint:
- Femoroacetabular Impingement (FAI) — Subtle shape differences in the ball (femoral head) or socket (acetabulum) can cause abnormal contact, leading to pain, stiffness, labral tears and eventual cartilage wear. FAI surgery aims to reshape bone and protect the labrum and cartilage. Learn more: FAI overview and hip osteoarthritis.
- Labral tears — The labrum is a rim of cartilage that seals the socket and stabilises the joint. Tears commonly occur with FAI or shallow sockets (dysplasia). We may repair or debride the labrum depending on tissue quality and stability requirements.
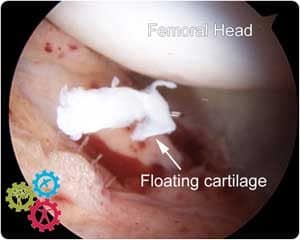
- Cartilage damage — Unstable cartilage flaps can be smoothed (chondroplasty). In select cases we use microfracture techniques to stimulate a protective fibrocartilage fill in small focal defects.
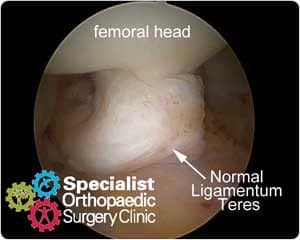
- Ligamentum teres tears — This cord-like ligament connects the ball to the socket. Depending on the pattern, we may debride, stabilise with radiofrequency, and consider image-guided injections as part of your plan.
Related pages: Physiotherapy · Anterior hip replacement · FAQs

How hip arthroscopy is performed
Hip arthroscopy may be performed as a day procedure; however, many patients benefit from one night in hospital for nursing care, pain optimisation and physiotherapy.
- Positioning & traction: You are positioned to allow gentle traction on the leg, creating space inside the joint for safe instrument passage.
- Incisions: We make 2–3 small incisions (≈1 cm) around the hip to insert the camera and instruments.
- Treatment: Depending on findings, we may perform labral repair, bone reshaping for FAI, cartilage smoothing, microfracture, and ligamentum teres treatment.
- Duration: The operation typically takes 30–90 minutes, guided by the complexity of your pathology.




After the Hip Arthroscopy
After surgery, you will wake in Recovery and then transfer to the ward. Our nursing team will monitor your pain control, comfort and early mobilisation. Many patients feel less pain than expected and can begin guided exercises the same day.
- Pain control: Regular simple analgesia and ice help manage early inflammation.
- Physiotherapy: A physiotherapist will teach early mobility, gait with crutches and gentle range-of-motion work.
- Discharge: Most patients go home the following morning with a personalised rehabilitation plan. See our physiotherapy pathway.
Recovery after Hip Arthroscopy
Most people go home the morning after surgery. Plan time off to allow swelling to settle and gait to normalise.
- Time off work: Office work 1–2 weeks; manual/strenuous roles 4–6 weeks (individualised).
- Return to activity (typical guide):
- Weeks 1–2: protected weight-bearing with crutches as advised.
- Week 4: stationary cycling, pool work as wounds permit.
- Week 6: progressive treadmill walking; begin light jog when strength and mechanics allow.
- Physiotherapy: For best results, work with our physiotherapy team skilled in hip prehab and post-arthroscopy rehabilitation.
When to contact us urgently
- Increasing redness, warmth or discharge at wounds
- Fever or chills
- Calf pain/swelling, chest pain or shortness of breath
Complications of Hip Arthroscopy
Complications are uncommon, but any operation carries risks. We weigh potential benefits against potential risks for your specific circumstances.
- Nerve irritation or injury: Rare, usually temporary. Nerves potentially affected include the lateral femoral cutaneous (outer thigh sensation), pudendal (from traction positioning) and sciatic. Symptoms can include numbness, tingling or pain.
- Infection: Very uncommon with modern sterile techniques but always a consideration; treatable if detected early.
- Persistent or recurrent pain: Relief depends on underlying cartilage health and associated conditions. Recovery is progressive, with most gains in the first 3 months; final outcomes can take up to 12 months.
- Adhesions (scar tissue): The hip capsule heals after surgery; occasionally scar tissue can tether the labrum, causing stiffness or pain. Physiotherapy protocols aim to reduce this risk.
- Clots (DVT/PE): Low risk; we assess individual risk factors and may prescribe preventative measures.
FAQs
What are the alternatives to hip arthroscopy?
We prioritise non-operative care first where appropriate: activity modification, targeted physiotherapy, anti-inflammatory strategies, and image-guided injections when indicated. If symptoms persist or function is limited, surgery may help.
When should I consider surgery?
Earlier intervention for mechanical problems (e.g., FAI with labral tear) can help protect the labrum and cartilage. Many patients experience better outcomes when treated before prolonged symptoms and secondary joint degeneration. Timing is individualised after clinical assessment and imaging.
[h4]How do I prepare for hip arthroscopy?[/h4]
Tests
You may need:
- Hip X-rays
- MRI (labrum & cartilage)
Most patients do not require blood tests or an ECG. Your hospital pre-admission questionnaire is reviewed by nurses and the anaesthetist; we will contact you if further checks are needed.
Skin & Support
Please ensure your skin is free of infection/irritation. Arrange help at home for meals, shopping and transport for the first 1–2 weeks.
Home Setup
- Remove trip hazards (loose rugs, cords)
- Use a stable chair with arms and a firm seat
- Consider a shower chair and long-handled sponge
What is normal after surgery?
Mild discomfort, bruising and swelling around the groin, thigh, lower back and buttock are common and settle with time. Some patients notice temporary numbness or tingling in the leg, foot or groin due to traction positioning—this usually resolves.
When can I walk and drive?
Most people walk with crutches the next day as comfort allows. Avoid driving for at least 48 hours after anaesthetic and until you can safely control the vehicle. Many patients resume short drives at around 1 week.
Do I need to change the dressing?
Dressings are usually secure and sealed with skin glue. Some oozing can occur in the first 24–48 hours. If a dressing lifts, you may replace it with a clean, dry one.
Next Steps
Next steps: If you have mechanical hip pain or suspected FAI/labral tear, book an assessment. We will confirm your diagnosis and map a non-operative or operative plan tailored to your goals.
Further Reading and References
- Basic Hip Arthroscopy: Diagnostic Hip Arthroscopy. Stone AV, et al. Arthrosc Tech. 2017;6(3):e699–e704.
- Danish Hip Arthroscopy Registry: outcomes in FAI. Lund B, et al. J Hip Preserv Surg. 2017;4(2):170–177.
- The current situation in hip arthroscopy. Marin-Peña O, et al. EFORT Open Rev. 2017;2(3):58–65.
- Hip pathology with normal imaging: arthroscopic findings. Buikstra JG, Fary C, Tran P. BMC Musculoskelet Disord. 2017.
