Trochanteric Bursitis (GTPS) – Overview
Trochanteric bursitis is a common cause of pain on the outside of the hip. It sits within the umbrella of Greater Trochanteric Pain Syndrome (GTPS), which also includes gluteal tendinopathy (typically involving the gluteus medius/minimus tendons) and irritation of the iliotibial band.
Most patients respond well to conservative care such as targeted physiotherapy, activity modification, anti-inflammatory strategies, and image-guided injections. In persistent cases with mechanical irritation or tendon pathology, endoscopic surgery (e.g., trochanteric bursectomy and selective iliotibial band release) may be considered after non-operative options have been exhausted.
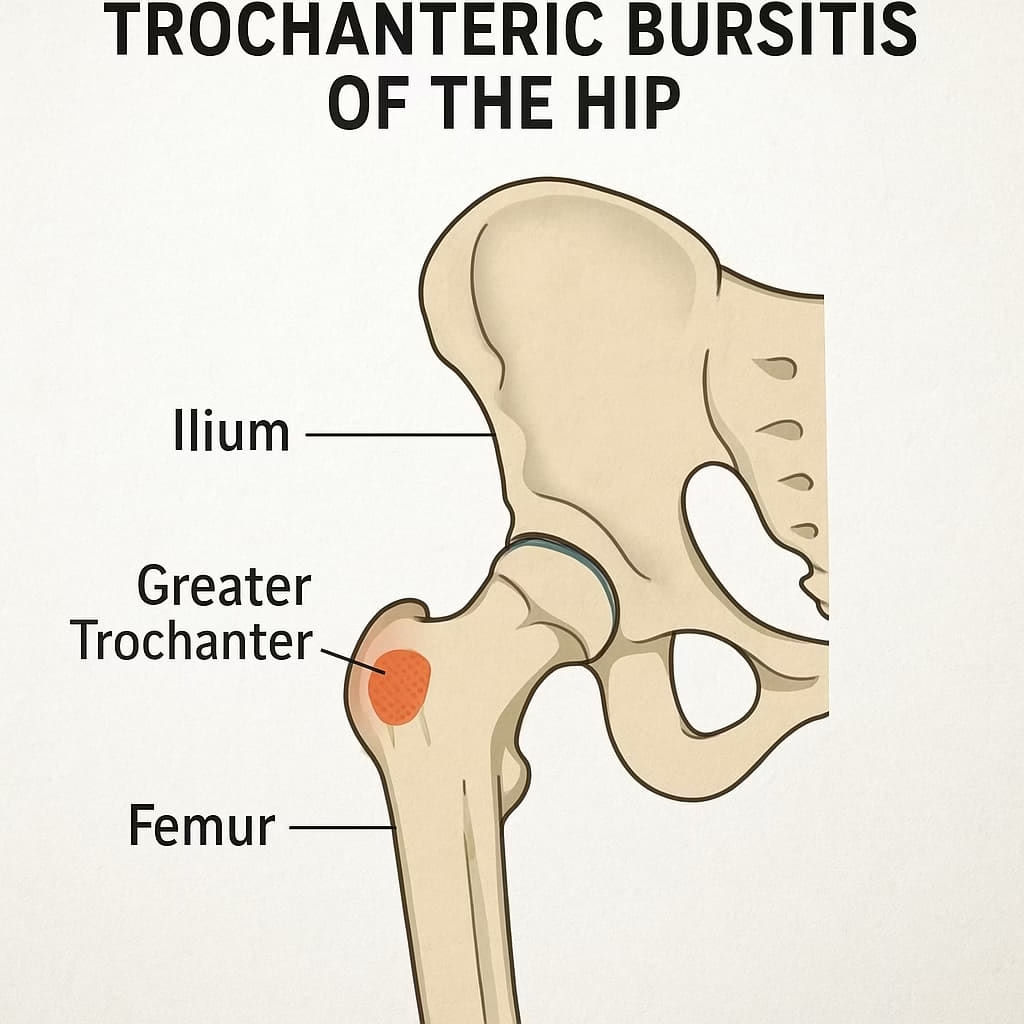
What is Trochanteric Bursitis?
A bursa is a fluid-filled sac that cushions and reduces friction between tendons, muscles, and bone. Several bursae exist around the hip, but the trochanteric bursa, located over the greater trochanter (outer hip), is most commonly irritated.
Bursitis occurs when the bursa becomes inflamed due to overload, repetitive friction, direct pressure, or secondary to adjacent hip pathology. Patients typically describe a dull, burning pain on the lateral hip that can radiate down the thigh. Night pain is common, especially when lying on the affected side.
Symptoms and Diagnosis
Diagnosis is clinical and based on history and examination. Typical features include:
- Pain and tenderness directly over the greater trochanter
- Discomfort with prolonged standing, walking, or stair climbing
- Difficulty sleeping on the affected side; pain with side-lying
- Trendelenburg pattern or limp in more severe cases
Imaging: X-rays help exclude intra-articular causes (arthritis, bony morphology). Ultrasound or MRI can identify bursal inflammation and coexisting gluteal tendinopathy or partial tears.
Conservative Treatment (First-Line)
Most patients improve with non-surgical management coordinated with our physiotherapy team:
- Load management & activity modification: temporary reduction of aggravating activities (e.g., prolonged side-lying on hard surfaces, steep hills, cambered footpaths).
- Physiotherapy: progressive strengthening of gluteus medius/minimus, lumbopelvic control, gait retraining, and ITB soft-tissue strategies.
- Pain relief: short courses of NSAIDs (if suitable), ice, and sleep positioning advice (pillow between knees to reduce compression).
- Injections: ultrasound-guided corticosteroid for short- to medium-term relief in irritable presentations; PRP may be considered in tendinopathy-dominant cases.
- Shockwave therapy (ESWT): can be adjunctive for chronic gluteal tendinopathy/GTPS when exercises alone plateau.
Time course: meaningful improvement commonly occurs over 6–12 weeks with adherence to a structured program.
Surgical Options (When Symptoms Persist)
For recalcitrant cases after comprehensive non-operative care, we may consider:
- Endoscopic trochanteric bursectomy: removal of inflamed bursal tissue through small keyhole incisions.
- Iliotibial band (ITB) release: selective release to reduce friction/compression over the greater trochanter.
- Gluteal tendon procedures: debridement or repair if significant tendinopathy or partial tears are confirmed.
These procedures are performed arthroscopically/endoscopically with the goal of pain reduction and function restoration. For details on minimally invasive technique and recovery principles, see hip arthroscopy.
Self-Care & Recovery Tips
- Sleep on the non-painful side with a pillow between knees to reduce compression.
- Gradually increase walking distance on flat surfaces; avoid steep inclines early.
- Use a cushion for hard chairs; avoid prolonged positions that provoke symptoms.
- Follow your physio-guided exercise plan consistently 3–4 times per week.
When to seek urgent review: fever, redness or warmth spreading from the hip, severe sudden pain after a fall, or neurological symptoms (new weakness, foot drop).
Further Reading and References
- The outcome of endoscopy for recalcitrant greater trochanteric pain syndrome. Drummond J, Fary C, Tran P. Arch Orthop Trauma Surg. 2016;136(11):1547-1554.
- Endoscopic Trochanteric Bursectomy and Iliotibial Band Release for Persistent Trochanteric Bursitis. Mitchell JJ et al. Arthrosc Tech. 2016;5(5):e1185-e1189.
- The management of greater trochanteric pain syndrome: A systematic literature review. Reid D. J Orthop. 2016;13(1):15-28.
FAQs
Is trochanteric bursitis the same as GTPS?
GTPS is an umbrella term that includes trochanteric bursitis, gluteal tendinopathy, and ITB-related friction. Many patients have a combination of these.
How long does recovery take without surgery?
With a structured exercise program and load modification, most people improve over 6–12 weeks. Some need an injection to settle pain so rehab can progress.
When are injections appropriate?
When pain is high or persistent despite exercises, an ultrasound-guided corticosteroid injection can reduce inflammation. PRP is sometimes considered for tendinopathy-dominant cases.
When should surgery be considered?
After thorough non-operative care has plateaued and imaging confirms ongoing bursal or tendon pathology, we may discuss endoscopic options.
What can mimic trochanteric bursitis?
Hip arthritis, lumbar spine referral, and FAI can present with lateral hip pain. Assessment and appropriate imaging help clarify the diagnosis.
Next Steps
Still sore on the outside of your hip? Book an assessment to confirm the diagnosis and start a personalised non-operative plan. If symptoms persist, we’ll discuss minimally invasive options.
